Our vision for smarter, kinder radiotherapy is that all appropriate patients will receive radiobiologically-guided and technically-exemplary reirradiation. Reirradiation may offer long-term cancer control but is currently not used extensively, due to limited understanding of fundamental biology and not-fit-for-purpose treatment technology. In Theme 2, we will address this by working to enhance our understanding of cancer cell and background tissue damage and recovery in the reirradiation setting, in order to maximise the benefits and minimise the side effects of reirradiation. We will link to local expertise in host immune response, to local and network expertise in DNA damage and repair, and to network expertise in circulating DNA for monitoring tumour and normal tissue response. We will thereby refine patient selection, drive development of new treatment strategies, and continue to develop and implement novel software solutions for highly individualised reirradiation treatments that maximise the therapeutic ratio. This will will build on our pioneering and internationally-recognised CRUK-funded work on personalised reirradiation treatment optimisation and ongoing multicentre reirradiation trials.
Theme Leads
Dr Louise Murray (Co-Lead)

Associate Professor, Clinical Oncology
Staff Profile: Dr Louise Murray | School of Medicine | University of Leeds
I am an Academic Clinical Oncologist. My PhD, completed here in Leeds, focused on technical radiotherapy for prostate cancer. This involved radiotherapy treatment planning, normal tissue complication probability, tumour control probability and second malignancy risk estimations.
My research interests include re-irradiation (delivering radiotherapy to a previously irradiated region), the implementation of modern imaging technologies in the radiotherapy treatment planning pathway, radiotherapy for brain and pelvic malignancies, the appropriate implementation of new technologies into the radiotherapy clinic and patient reported outcomes in response to radiotherapy.
Professor Adel Samson (Co-Lead)

Professor of Cancer Medicine and Immunotherapy; Consultant Medical Oncologist
Staff Profile: Professor Adel Samson | School of Medicine | University of Leeds
I am a Professor of Cancer Medicine and Immunotherapy and a Consultant Medical Oncologist specialising in the treatment of liver cancers. My research spans multiple key steps in clinical immunotherapy development, including pre-clinical laboratory conceptualisation and optimisation, early phase clinical trials, and translational studies using clinical trial samples. My laboratory group focuses on harnessing the immune system to treat solid malignancies, optimising the efficacy and delivery of immunotherapies to tumours, and understanding the immunological effects of radiotherapy, histotripsy and oncolytic virus therapy. As Chief or Principal Investigator, I lead a portfolio of translational clinical trials focused on oncolytic viruses and liver cancers.
Dr Ane Appelt (Co-Lead)

Associate Professor, Radiotherapy Physics
Staff Profile: Dr Ane Appelt | School of Medicine | University of Leeds
I am a cancer researcher, clinical trialist, and medical physicist. My research focuses on improving patient outcomes through the development and implementation of optimised treatment strategies and novel technological innovations in radiotherapy. My interests include reirradiation, radiotherapy for organ preservation, clinical trial design and delivery, and the application of data science in radiation oncology. I am a strong advocate for research that is both clinically relevant and translatable into practice. This includes a core belief in the importance of clinical trials as a critical means for evaluating radiotherapy innovation. I lead a competitively funded, multicentre, randomised dose-escalation trial in rectal cancer and am involved in over a dozen other trials. I am primary or co-investigator on active grants totalling over £5.6 million.
As well as co-leading Theme 2, I am the co-lead for RadNet Leeds Theme 1 Work Stream 2, which applies federated and deep learning to multimodal radiotherapy data for outcome prediction and treatment optimisation.
Theme 2 emerging leaders
Dr Qian Wu

Group Leader, DNA repair, DNA damage response, BRCA1, DNA repair pathway choice, structural biology
Staff Profile: Dr Qian Wu I Faculty of Biological Sciences I University of Leeds
My group is studying the fundamental mechanism of how cells respond and deal with DNA damage. Human cells are under constant threat of damage from external and internal sources. One of the most dangerous forms of damage is to DNA. Accumulated DNA damages lead to cell death and genome instability, which can cause cancer, neurodegenerative disease and ageing. Maintaining the integrity of genetic information stored in DNA through various damage response and repair signalling pathways are critical for cellular function and cell survival. We focus on the structural determination of key protein complexes function in DNA damage response (DDR) and repair. Together with various biochemical/biophysical methods and cellular studies, we would like to work out the exact mechanisms in human DDR and repair network.
Research interests
We study DNA double-strand breaks (DSBs), which are the most toxic damages in cells. Through our research, we would like to identify suitable targets to develop small molecule compounds that modulate the DNA damage response and repair signalling for future drug discovery, medical applications and ultimately killing cancer cells specifically.
Mr Christopher Thompson

Principal Clinical Scientist
I am a RadNet Principal Clinical R&D Scientist, having worked in radiotherapy since 2002. I have been active in research for a number of years with a focus on reirradiation treatment planning. After successful work on novel treatment planning tools for reirradiation in collaboration with commercial partners, this will continue to be a focus of RadNet. I am also working on deformable image registration and robustness tools both key requirements for the reirradiation planning implementation.
In my clinical role at Leeds Teaching Hospitals NHS Trust, I support evaluation and implementation of external beam developments, leading the implementation of complex treatment techniques including paediatric planning.
Dr Finbar Slevin

Honorary Clinical Consultant
Staff Profile: Dr Fin Slevin I School of Medicine I University of Leeds
Fin is an honorary consultant in clinical oncology and future leader at Cancer Research UK RadNet Leeds. He commenced a five-year NIHR Advanced Fellowship in April 2025. MAPP-RT (Modelling and Patient Perspectives to optimise Pelvic Radiotherapy) will see Fin collaborate with multidisciplinary radiotherapy teams from Leeds and Manchester to analyse radiotherapy planning and toxicity data from multiple clinical trials of pelvic radiotherapy in prostate cancer. This work will evaluate spatial relationships between the radiation dose received by normal tissues and development of toxicity. Combined with qualitative research to understand patients’ perspectives, MAPP-RT will enable Fin to develop, implement and evaluate novel methods for pelvic radiotherapy planning which aim to minimise risk of toxicity. The project is strongly aligned with Theme 1 Personalised and Adaptive Radiotherapy and, through its use of clinical trial data in recurrent prostate cancer, will support reirradiation research in Theme 2. To read a Plain English Summary of Fin’s research and to follow updates, see his Fellowship webpage.
Workstream 3 – Re‑irradiation biology
Focus on reirradiation biology in brain, liver and pelvic cancers
We aim to understand drivers of tumour, normal tissue and host response to reirradiation, to guide patient
selection and development of new, smarter, kinder treatment strategies. The Workstream leads are Professor Richard Bayliss, Professor Adel Samson and Dr Qian Wu, and they aim to answer four key questions:
- What characterises DNA, tumour, normal tissue, and host response to reirradiation; can this be used to develop novel treatment strategies?
- Is there a differential host immune response to reirradiation compared to de novo irradiation?
- Can circulating tumour and normal tissue DNA be used to monitor response and toxicity to reirradiation?
- What is the optimal statistical methodology for modelling complex radiotherapy data to understand normal tissue response and recovery?
Professor Richard Bayliss

Professor of Cancer Biology
Staff Profile: Professor Richard Bayliss I Faculty of Biological Sciences I University of Leeds
Our research aims to understand the molecular mechanisms that cause disease and to develop new or improved therapies. We research the protein kinases associated with cancer signalling pathways, the transcription factor Myc, the assembly and function of the spindle assembly, proteostasis and structure-based approaches to drug discovery. We also have interests in synthetic biology, microcephaly and in kinases associated with infectious disease.
Workstream 3 key collaborator:
Professor Steve Jackson, University of Cambridge

Cancer Research UK Cambridge Institute
University of Cambridge Department of Biochemistry
Staff Profile: Professor Steve Jackson I Department of Biochemistry I University of Cambridge
Workstream 4 – Bringing novel re-irradiation to the clinic
Focus on brain, liver and pelvic tumours
We will develop and evaluate innovative, smarter, kinder treatment strategies and technologies for reirradiation,
implemented through existing trials and a new pilot study, while supporting underpinning biology through a
strong translational focus. Workstream 4 leads are Dr Louise Murray and Dr Ane Appelt, who will:
- bring novel EQD2-based reirradiation treatment optimisation into the clinic using existing studies (Ro-PIP, POINTER-PC).
- determine whether reirradiation treatment planning and delivery be made robust to radiobiology and image registration uncertainties.
- perform a liver reirradiation pilot study combining isotoxic planning, functional imaging and radiobiological, anatomical, and treatment uncertainties into plan optimisation.
- through ongoing trials (Ro-PIP, POINTER-PC, BRIOChe) and the liver reirradiation study, we will contribute imaging & translational samples to WS3, and establish high-quality, multi-modal, longitudinal datasets to support radiobiological modelling.
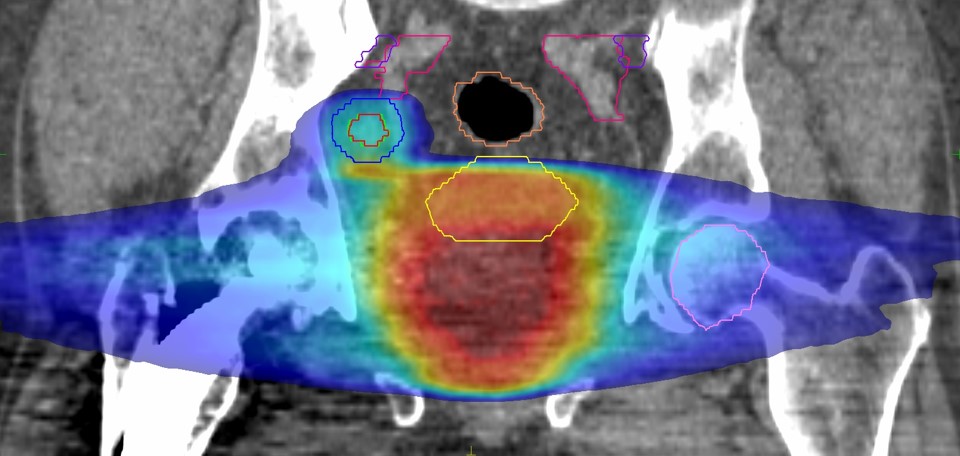
Combined radiotherapy dose distribution for patient coming back for re-treatment of a lymph node recurrence after initial radiotherapy for prostate cancer.
