Theme 2 aims to transform the use of re-irradiation. We will develop re-irradiation strategies tailored to the individual patient, incorporating radiobiology, anatomical changes, and multi-modality imaging, and take these strategies into the clinic in pilot studies in rectal and prostate cancer.
Theme Leads
Dr Louise Murray (Co-Lead)

Associate Professor, Clinical Oncology
Staff Profile: Dr Louise Murray | School of Medicine | University of Leeds
Dr Ane Appelt (Co-Lead)

Associate Professor, Radiotherapy Physics
Staff Profile: Dr Ane Appelt | School of Medicine | University of Leeds
Work Package 3 – Re‑irradiation – Combining imaging with radiobiology
Work package 3 will create methodology, technical solutions and data analysis strategies for re-irradiation. We will combine prior dose distribution, state-of-the-art deformable image registration, and radiobiology, as well as pre-treatment functional imaging to identify sub-clinical damage from previous radiotherapy, to guide safe re-irradiation and assess toxicity following treatment.
Work Package 4 – Taking novel re-irradiation into the clinic
Work package 4 will take the solutions from WP3 into the clinic, as pilot studies in rectal and prostate cancer. These studies will focus on neo-adjuvant re-irradiation in recurrent rectal cancer, primary prostate re-irradiation in localised castrate resistant locally recurrent prostate cancer, and pelvic SABR and elective nodal irradiation for pelvic oligometastatic disease.
Other WP4 Researchers
Mr Aaron Quyn

Associate Professor, Colorectal Surgery
Staff Profile: Meet the Team – NIHR Surgical MedTech Co-operative
Dr Alex Gilbert

Honorary Consultant and Senior Clinical Trials Fellow
Staff Profile: Dr Alex Gilbert I School of Medicine I University of Leeds
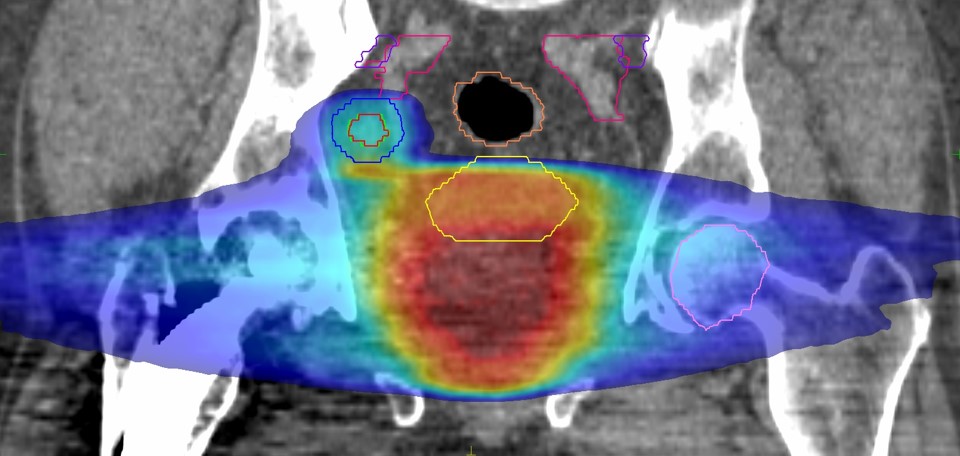
Combined radiotherapy dose distribution for patient coming back for re-treatment of a lymph node recurrence after initial radiotherapy for prostate cancer.
